Disease-related malnutrition is a condition in which patients are not getting the right nutrition in the right amount to sustain their health. According to World Health Organisation (WHO) and European Society for Clinical Nutrition and Metabolism (ESPEN), patients affected by disease-related malnutrition are:
- 3.4x more likely to die
- stay 1.9x longer in hospital and
- 2.2x more prone to comorbid conditions such as infections and ulcers.1
Furthermore, the estimated cost to our economies in the European Union reaches €120 billion — and up to €170 billion across Europe2.
“Although it is increasingly clear that nutritional care can effectively prevent or treat malnutrition and improve disease outcomes,” while also providing economic benefits, “access is still unacceptably limited for most patients.”1
The evidence shows that disease-related malnutrition is a widespread, yet preventable health challenge that worsens patient outcomes, drives up healthcare costs and deepens inequalities across health systems - MEP Vytenis Andriukaitis
The barriers to equity
A survey conducted by the Medical Nutrition International Industry (MNI) across ten European countries from different regions reveals major differences in how disease‑related malnutrition is identified and addressed.
The latest MNI white paper “Towards closing inequity gaps in access to medical nutrition: Understanding the barriers” highlights that:
- While screening for malnutrition is available in 80% of countries surveyed, it is mandatory only in 20 %.
- Strengthening education for healthcare professionals is essential, given that only one country reported comprehensive knowledge of nutritional care, while in 78% of countries expertise varied by medical specialty and was predominantly limited to hospital settings.
Although most countries (90 %) reported some level of reimbursement for Food for Special Medical Purposes, coverage still varies by setting, condition and age, contributing to inequity of access to nutritional interventions3.
We must adopt standardised policies to ensure systematic malnutrition screening and fair access to nutritional care across the EU - MEP Vytenis Andriukaitis
A call for policy action
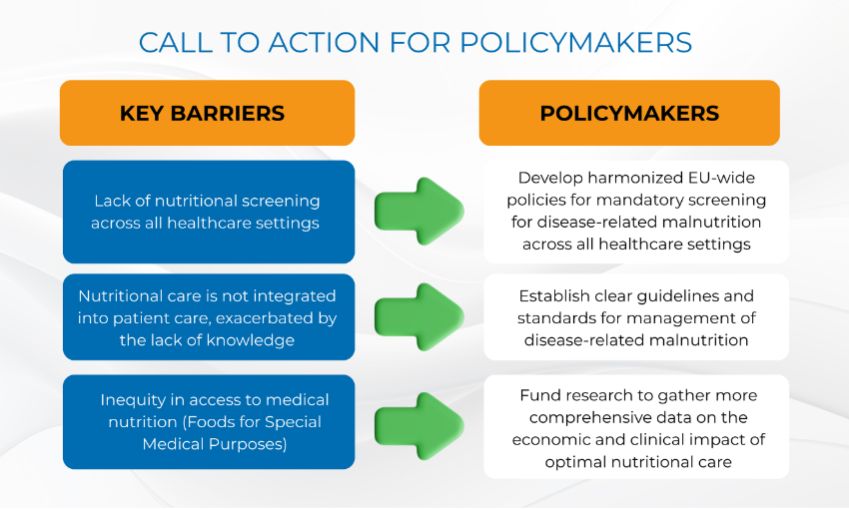
Policymakers have a crucial role to play to ensure that all patients across the EU have access to nutritional interventions. The white paper urges policies requiring nutritional screening in all healthcare settings, clear guidelines and standards for managing malnutrition, and funding for research on the economic and clinical benefits of optimal nutritional care.
Medical nutrition represents “a cost‑effective intervention that delivers both clinical and financial benefits” and, given its proven positive effects on patients’ clinical outcomes and quality of life, should not be viewed as treatment only for a few.
List of references
- https://iris.who.int/server/api/core/bitstreams/5d787241-5978-46d4-802e-44aeadf1d98d/content
- https://www.medicalnutritionindustry.org/content/uploads/2023/10/2018_mni_dossier_final_web.pdf
- https://www.medicalnutritionindustry.org/closing-inequity-gaps/
Sign up to The Parliament's weekly newsletter
Every Friday our editorial team goes behind the headlines to offer insight and analysis on the key stories driving the EU agenda. Subscribe for free here.